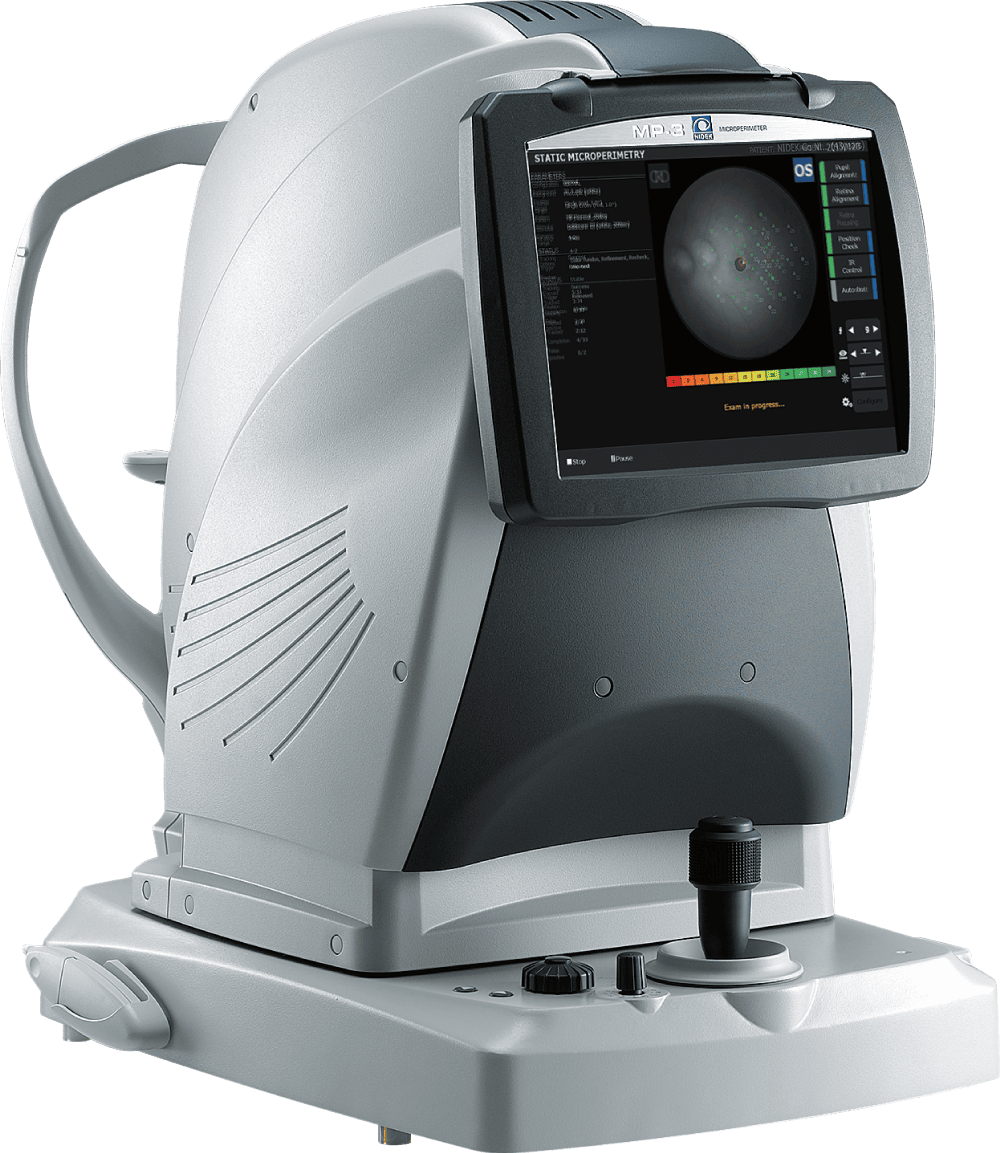
A Case Study on the MP-3 in a Retina and Low Vision Practice
BACKGROUND/PURPOSE
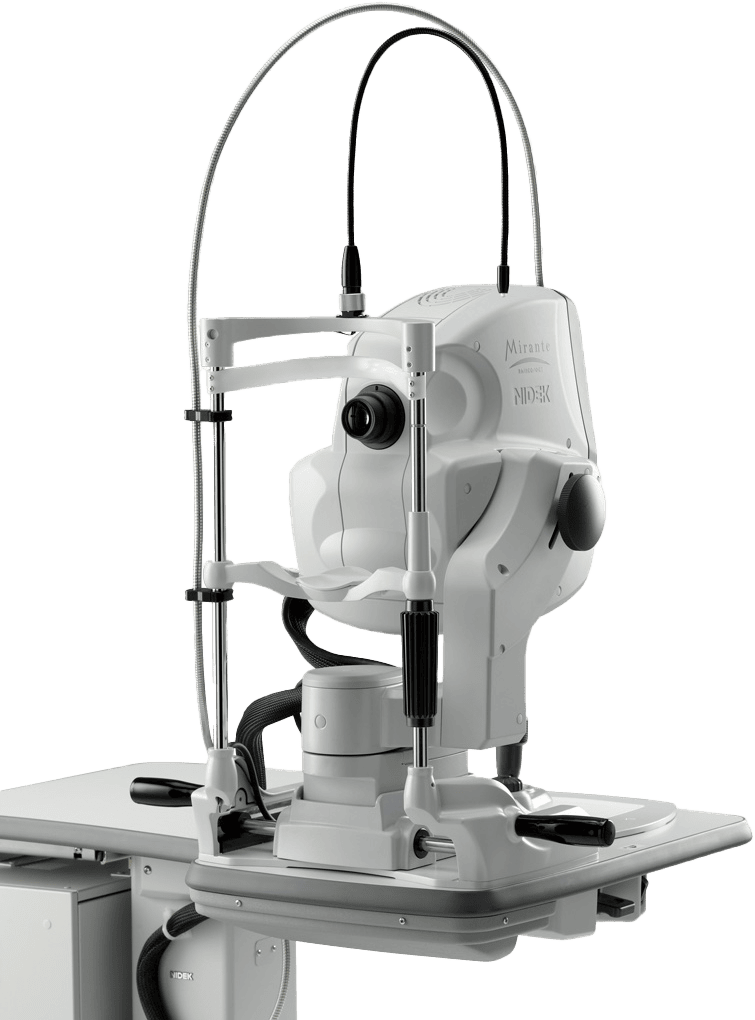
Central vision loss can be caused by congenital or acquired retinal disease including ARMD. Our retinal doctors at MOORE EYE INSTITUTE treat the retinal disease and the patient’s functional needs are treated during the low vision evaluation. One method of achieving clearer vision is to enlarge the image through magnification both at distance and near but the field of vision will also be reduced. Some patients are able to eccentrically view around the central loss but it is still difficult for them to locate the preferred retinal loci (PRL) and even more difficult to consistently find it. The purpose of this study with the NIDEK MP-3 is to identify the best eccentric viewing posture in ARMD patients and rehabilitate these patients to locate it consistently with the biofeedback training. This treatment plan allows the patient to be seen by their low vision optometric specialist and the retinal doctor without any additional therapists or traveling to any other locations.
METHODS
Each participant received a complete ocular examination including visual acuity (Snellen and SOSH low vision chart), retinoscopy and ophthalmoscopy. For those patients treated with injections for wet ARMD, the patient had to have no evidence of retinal active findings (SMR, SRF or heme) for at least three consecutive months. The ophthalmic technician performed an initial baseline retinal sensitivity analysis on the NIDEK MP-3.
Various light intensities are presented on the MP-3 and the patient responds with a clicker, similar to what is used on standard visual field test equipment. Stimulus intensity is measured in decibels (0-34). A high score indicates the patient’s ability to detect a dim stimulus and therefore a higher or better retinal sensitivity. A low score signifies poor sensitivity and manifests as a scotoma.
In the examination room, a low vision optometrist determined an eccentric viewing posture using a clock dial technique. It is an arduous process and has inconsistent results. The MP-3 can be used with these clock dial results to support them or it can locate the retinal position of preferred eccentric viewing independently. It is far more accurate, less time consuming and easier for the patient to be tested on the MP-3. Many patients had previously undergone OCT and Swept Source OCT. The retinal specialist compared the OCT with the MP-3 to check if they correlated. The sensitivity results can be documented and the rehabilitation process will be much more valid. After an eccentric viewing posture is determined, the low vision specialist delineated the area on the MP-3 for these patients to be trained to eccentrically view to that position. They receive auditory feedback when they locate the previously documented point. The patient was asked to move fixation to the trained area, then a flickering checkerboard in the trained area was presented and the patient was instructed to look away, and then have to locate the predetermined area of trained fixation. When the patient was successful, a constant beep would sound – the auditory feedback. This process was repeated several more times when the patient would look away and have to locate it on their own.
RESULTS/DISCUSSION
Our test participants consisted of 50 ARMD patients currently seeing doctors in the practice and who were willing to perform the MP-3 visual field test. We encountered many variables: visual acuity, cognitive ability, the duration, and severity of retinal disease and the ocular media. After 100 trials of the test, it was concluded our most successful patients had very reduced acuity in one eye (worse than 20/400) and moderately reduced acuity in the other eye (worse than 20/70). It was determined that their ability to understand the test also affected their performance on the biofeedback component. The patient needed to associate the auditory confirmation with the eccentric viewing posture. The challenges on repeated testing were financial, transportation and desire. Previously patients with central vision loss were taught by therapists to eccentrically fixate over many visits. The MP-3 accomplishes this in the doctor’s office, without the variability of different examiners and is far more efficient for the patient.
The benefit of this test is that the results are reproducible. They can be repeated on the same retinal location at different times to measure long term retinal function and correlate that with structural changes. The entire process can be completed in 10 minutes. Standard visual acuity measurements are not an accurate method of monitoring reduced central vision loss. Although the visual acuity may not have improved with many of the patients, it remained stable and their ability to return to the eccentric viewing posture was constant. Another less obvious advantage to the MP-3 testing is the psychosocial component. ARMD patients often feel they are not in control of their ocular prognosis. This procedure builds their confidence and they feel they are involved in their functional improvement. The NIDEK MP-3 provides the optometrist, low vision specialist, and the retinal doctor with the valuable data regarding the progression and rehabilitation of this disease. It is an accurate, efficient, and reliable piece of equipment to include in all offices.
CONTRIBUTORS at Eye Moore Institute in Pennsylvania
- Georgia Crozier, OD, MS
- Leonard Ginsburg, MD
- Shyam Kodati, MD
- Deepaki Malik, MD
- William Davis, COA
For more info about the NIDEK MP-3 Microperimeter, visit: https://usa.nidek.com/mp-3